January is Cervical Health Awareness Month

January is Cervical Health Awareness Month. The World Health Organization has a plan for the elimination of cervical cancer through vaccination and screening—we can get there! This January, we encourage you to learn more about cervical health and cervical cancer prevention and take steps to help eliminate this preventable cancer. Below are resources from our program, the National Cervical Cancer Coalition (NCCC).
Get Involved—Download the Toolkit for Advocates
Get Educated with Project PEACH
Listen to the Cervical Cancer Survivor Series
Check in with a Local NCCC Chapter
NCCC volunteer chapter leaders—many of whom are cervical cancer survivors—are passionate about seeking out opportunities to educate people in their local communities. They bring a true passion to help others and have reached thousands of people across this country through their efforts. You can check here to see if you have a local chapter and see what plans the chapter has for January.






Promote Cervical Health on Social Media
You can help ASHA and NCCC promote the importance of cervical health and cervical cancer prevention by sharing prevention messages throughout the month that cervical cancer is preventable! In addition to the messages below, you can check out the NCCC Ambassador Toolkit for additional graphics and posts to share.

- January is Cervical Health Awareness Month. Visit NCCC to learn more. Get involved and make a difference! http://ow.ly/MdJb30760xc
- During Cervical Health Month in January ASHA is offering free downloads of our fact sheets and a fotonovela. Get yours today. https://tinyurl.com/2p8hesrh
- During Cervical Health Month in January you can download free materials from NCCC. For more go to NCCC. Get involved, make a difference! https://www.nccc-online.org/cervical-health-awareness-month/
- Not one single woman ever needs to die from cervical cancer. We have the tools we need to prevent this disease so let’s use them. Get involved. Make a difference! Visit the National Cervical Cancer Coalition online https://www.nccc-online.org/
- January is Cervical Health Awareness Month. Learn more, get involved, make a difference! http://ow.ly/g3RQ30760mz #CervicalHealthMonth
- Tons of free materials – fact sheets, a fotonovela, and more https://tinyurl.com/2p8hesrh #CervicalHealthMonth
- Find free/low cost Pap tests in your area. http://ow.ly/9REq30760to #CervicalHealthMonth
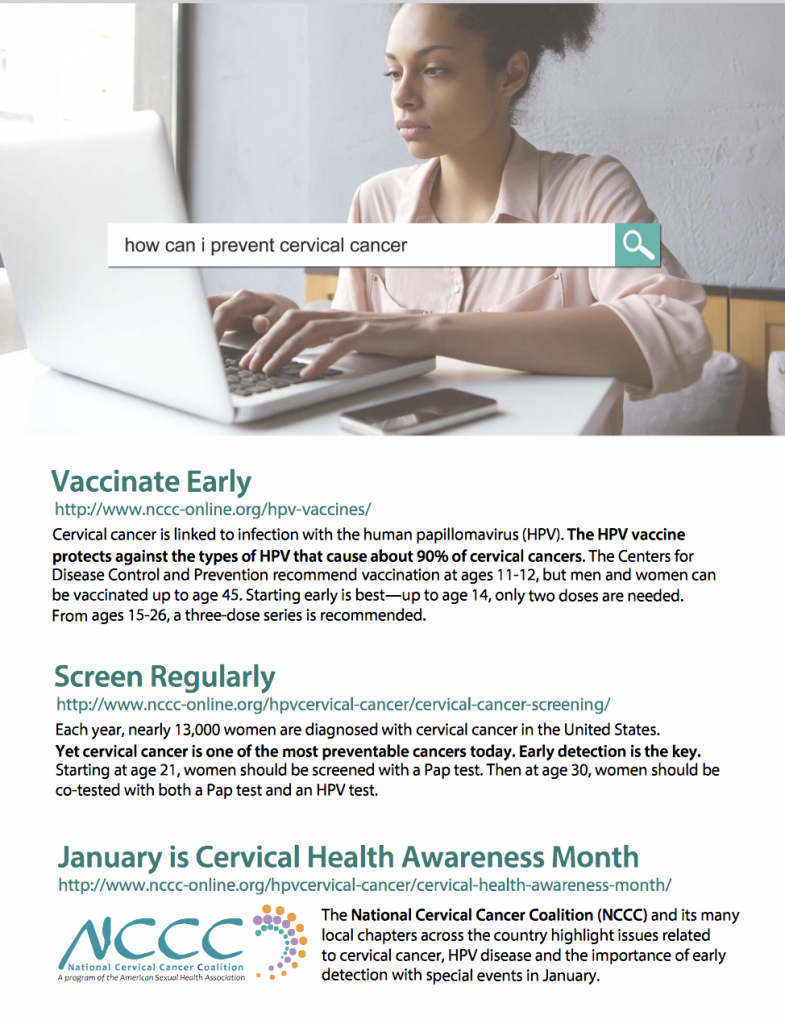
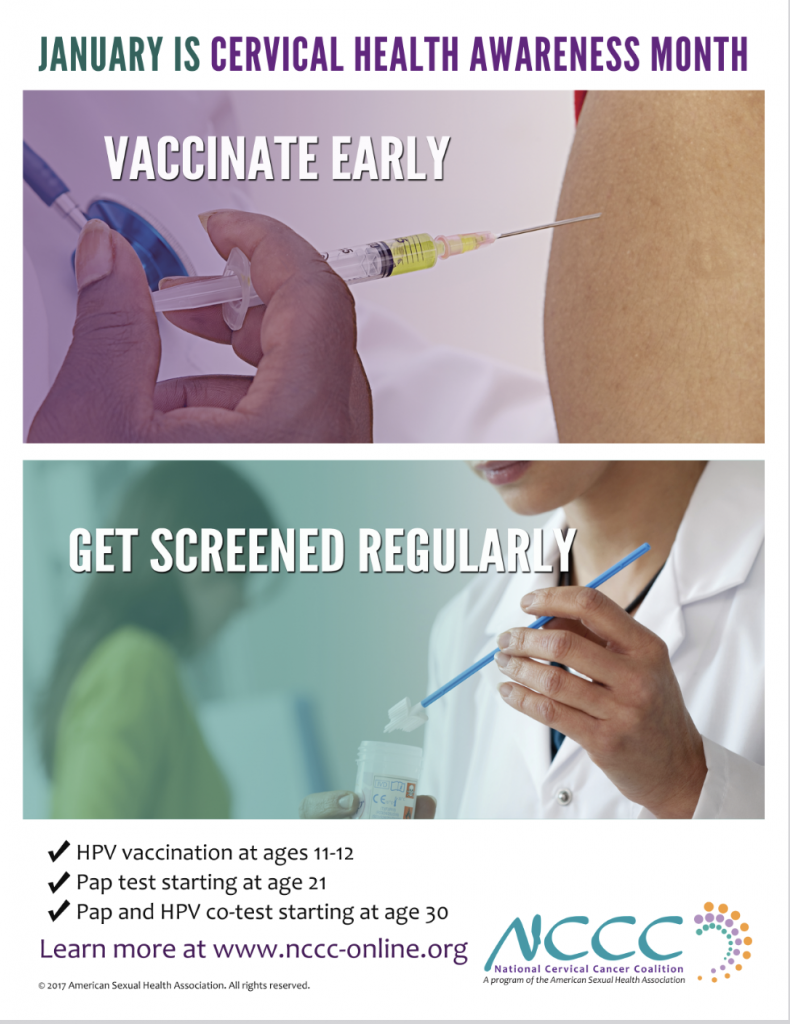
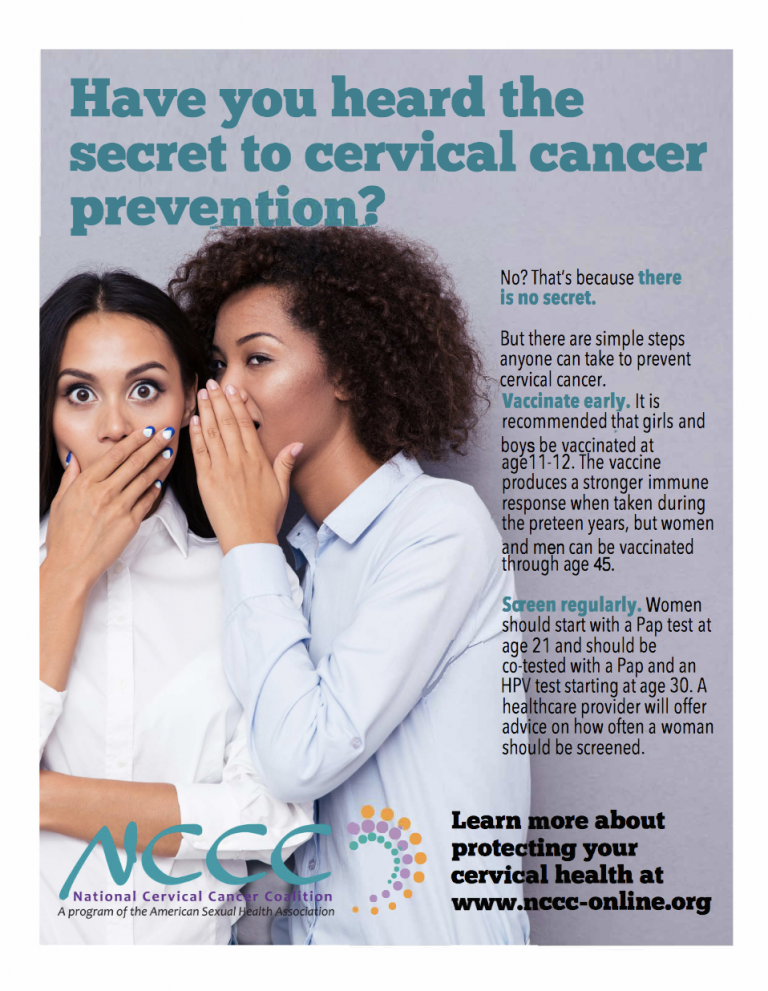
Download Content to Share
- Free ebook: HPV & Cervical Cancer: Stories from Survivors and Supporters
- Cervical Cancer Awareness Month Posters (click on an image to view and download)