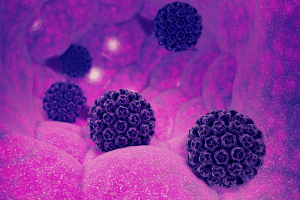
HPV and Relationships
HPV is one of the most common sexually transmitted infections. Still, finding out that you or your partner has it can feel stressful and confusing. It’s normal to have a lot of questions: What does this mean for our health? Did someone cheat? Should we