The name says it all. Long-acting reversible contraception, or LARC, is reversible birth control that provides long-lasting (think years) pregnancy prevention.
While not currently the leading choice among women, LARC use has been on the rise in recent years. In women aged 15-44, the rising popularity of LARC can likely be attributed to its high rate of effectiveness (more than 99 percent) and ease of use.
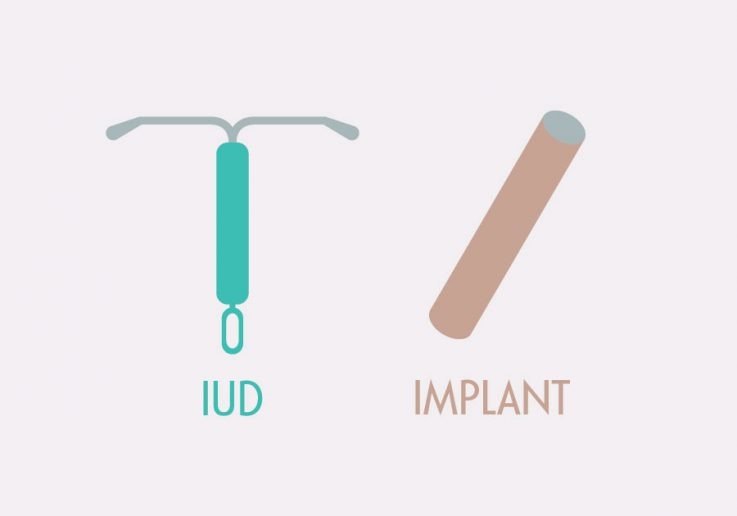
LARC methods—intrauterine devices (IUDs) and implants—are highly reliable. Research has shown LARC methods to be 20 times more effective than birth control pills, the patch, or the vaginal ring.
One important reason why is the LARC removes the “user error” factor that can make other methods less effective. No need to remember to take a pill daily, or have a diaphragm on hand ready to go. Once a LARC is in place, it does its job for years with no input from the user at all, acting as a “set it and forget it” method.
But there’s one thing that shouldn’t be forgotten—protecting against sexually transmitted infections (STIs). While LARC is a highly effective way to prevent pregnancy, LARC methods don’t provide any protection against STIs. For this reason, many people choose to use (and health professionals recommend) condoms in addition to a LARC method. Dual use of condoms and LARC offers dual prevention.
LARC Methods
There are two LARC methods: the intrauterine device (IUD) and the birth control implant. The intrauterine device (IUD) was once a popular choice in the U.S., but following problems linked to the poorly designed Dalkon Shield model in the 1970s, usage dropped due to concerns about safety. A new generation of IUDs was introduced in the early 2000s, and today’s models have none of the earlier safety concerns. But some misconceptions still persist.
The birth control implant has been available in the United States since the 1990s. The earliest model, Norplant, included multiple rods implanted under the skin on the inner arm. It offered pregnancy prevention for up to five years. While it was easy to insert, some people experienced problems with the removal procedure, and the manufacturer had issues finding the ingredients it needed to make the product.
Norplant was taken off the market in 2002, and a new generation of implants, now called Nexplanon, was introduced a few years later. This device consists of only one small rod, and both insertion and removal are easy.
The history of contraceptive implants is also complicated by coercive practices that emerged almost immediately after Norplant became available. Several states introduced legislation mandating its use in specific groups of women, including those receiving public assistance. In addition, some women facing court charges, such as child and abuse and neglect, were offered the option of accepting implants in exchange for a reduced sentence. Like so many coercive practices, Black and brown women were disproportionately impacted.
Understanding and acknowledging this history of coercive use of LARC and safety concerns is important, to avoid problems of the past. But so too is understanding the potential value of current LARC methods.